Inflammatory Bowel Disease: Causes, Symptoms, Diagnose and Treatment
Inflammatory Bowel Disease
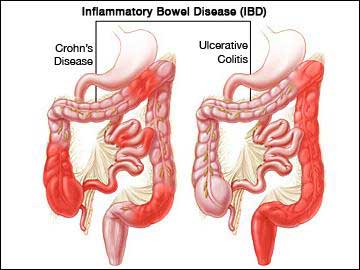
Inflammatory bowel disease can be divided into two chronic inflammatory disorders of the Gastrointestinal tract, namely Crohn’s disease (CD) and Ulcerative colitis (UC).
Inflammatory Bowel Disease
Crohn’s disease affects any part of the gastrointestinal tract whereas ulcerative colitis affects the colon and rectum only.
Ulcerative colitis (UC)
Currently, available treatment for IBD is not curative. IBD follows a relapsing and remitting course that is unpredictable and causes disruption to a patient’s lifestyle and places a burden on the workplace and
healthcare setting. The management of IBD patients poses a challenge to the multidisciplinary team both clinically and economically.
Incidence of IBD
The incidence of IBD is greater in north America, Europe, Australia and New Zealand, although the incidence in Africa, Asia, and South America is rising steadilyThis increase in developing countries may be due to improved sanitation and vaccination programs along with a decreased exposure to enteric
infections. The peak incidence of IBD occurs between 10 and 40 years, although it can occur at any age, with 15% of cases diagnosed in individuals over the age of 60 years. The incidence appears equal between
males and females, although some studies in Crohn’s disease show a slight female predominance.
Cause of Inflammatory Bowel Disease
The causative agents of IBD are large although a number of factors are
thought to play a role.
Environmental Factors:
It includes the following factors
Diet: Evidence that dietary intake is involved in the aetiology of IBD is inconclusive, although several dietary factors have been associated with IBD, including fat intake by the organism, fast food ingestion, milk and fibre consumption, and total protein and energy intake. During the course of the disease, patients are able to identify foods which aggravate or exacerbate their symptoms, for example, milk or spicy foods. Upto 5% of patients with
ulcerative colitis improve by avoiding cow’s milk, whilst the patient with Crohn’s disease improve if they start to elemental (amino acid base), oligomeric (peptides) and polymeric (whole protein) feeds, although
Symptoms may Recur when Patient Follows Normal Diet.
Smoking
There is a higher rate of smoking amongst patients with Crohn’s disease than in the general population, with up to 40% of patients with the disease being smokers. Former smokers are at the highest risk of developing ulcerative colitis, while smokers who continue to smoke have the least risk. In some studies nicotine has been shown to be an effective treatment for ulcerative colitis.
Infection
Exposure to Mycobacterium paratuberculosis has been considered a causative agent of crohn’s disease, although current evidence indicates it is an aetiological factor.
Enteric Microflora
This flora plays an important role in the pathogenesis of IBD because the gut acts as a sensitising organ that contributes to the systemic immune response. Persons with IBD shows less immunological tolerance to intestinal microflora and consequently antibiotics often play a role in the treatment of IBD.
Drugs
Non-Steroidal anti-inflammatory drugs (NSAIDS) such as diclofenac have been reported to exacerbate IBD.
Appendicectomy: Appendicectomy has a protective effect in both Crohn’s disease and ulcerative colitis. It is still unclear that this protective effect is immunologically based or whether individuals who develop appendicitis.
Stress
Some patients find that stress triggers a relapse in their IBD and this has been reproduced in animal models.
Genetic factors
15% of first degree relatives have IBD.
Ethnic and familial
Jews are more prone to IBD than non-jews, with Ashkenazi Jews having a higher risk than Sephardic Jews.
Clinical Manifestation (Symptoms)
The clinical feature of Crohn’s disease and ulcerative colitis are given below.
Crohn’s Disease
It depends largely on the site of bowel affected, the extent, severity and the pathological process in each patient. This disease tends to be more disabling than UC with 25% patients unable to work one year after diagnosis. Common symptoms are
- Diarrhoea
- Abdominal pain
- Weight loss
Ulcerative Colitis
- Typical symptoms of Ulcerative Colitis Include
- Bloody diarrhoea with mucus ( most predominant symptom)
- Abdominal pain with fever
- Weight loss in severe cases.
How One can Diagnose Inflammatory Bowel Disease(IBD)
Radiological, pathological and clinical investigations help to confirm diagnosis, disease recurrence and response to treatment.
Differential diagnosis of IBD include carcinoma, infection, drug-induced colitis, ischaemia, radiation damage, irritable bowel syndrome and diverticulitis.
- Endoscopy
- Radiology
- Laboratory findings
- Stool tests
- Clinical assessment tools
Treatment of Inflammatory Bowel Disease
At present there is no cure for IBD since the exact cause of the condition is unknown. A wide range of drugs and nutritional supplements are available to maintain the patient in long periods of remission in this condition.
Nutritional Therapy
It can be considered as primary treatment, although a potential problem for all patients with IBD, patients with crohn’s disease are at particular risk of becoming malnourished and developing a variety of nutritional deficiencies. Therefore, It is, important to receive optimal nutrition and dietary manipulation as needed.
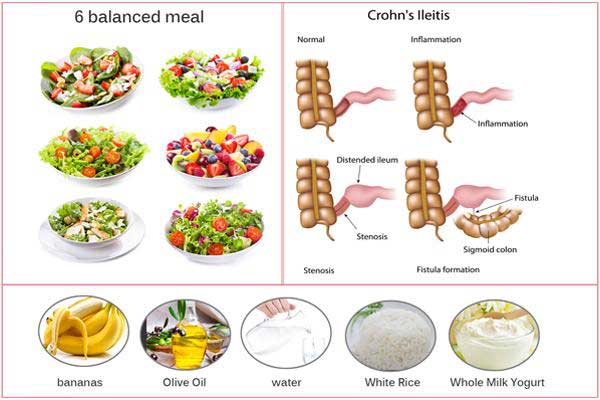
Nutritional Therapy
- Low-fibre diet help to reduce clinical symptoms of intestinal obstruction in Crohn’s disease.
- Low-lactose diet is also recommended.
- Total parenteral nutrition regimen is prescribed when there is inadequate nutrition.
Drug Treatment
The main goals of drug treatment are to treat acute attacks promptly and effectively, induce and maintain remission, limit drug toxicity, modify the pattern of disease, avoid complications and select patients who will benefit from surgery.
Corticosteroids, aminosalicylates and immunosuppressive agents such as azathioprine are the mainstays of treatment.
Other drugs such as antibiotics, for example, metronidazole, are helpful in some cases, while cholestyramine, thalidomide, bismuth and arsenical salts, nicotine, lidocaine, sucralfate, aloe vera, probiotics and fish oils are rarely used.
















































