Chronic Heart Failure: Symptoms, Causes, Diagnosis, Prevalence, Treatment, Patient Care
Chronic Heart Failure
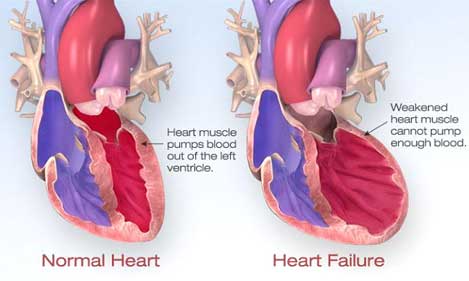
Chronic heart failure occurs when the heart unable to deliver an adequate amount of blood to the tissues and organs which result in inadequacy of oxygen and nutrients. Chronic heart failure is a complex condition associated with a number of symptoms arising from defects in left ventricular filling and/or emptying, of which shortness of breath, fatigue, and ankle swelling are the most common.
Chronic Heart Failure
Prevalence of Chronic Heart Failure
Chronic heart failure is a common condition with a prevalence ranging from 0.3% to 2% in the population at large, 3–5% of the population over 65 years old, and between 8% and 16% of those aged over 75 years. Heart failure accounts for 5% of adult medical admissions to hospital. There is a loss of cardiac reserve with age, and heart failure may often complicate the presence of other conditions in the elderly. More than 10% of patients with heart failure also have atrial fibrillation as a contributory factor. This combination presents a risk of thrombo-embolic complications, notably stroke; the risk is 2% in patients in sinus rhythm but may exceed 10% a year in patients with atrial fibrillation who are not anticoagulated and have attendant risk factors.
Causes of Chronic Heart Failure
The common underlying aetiologies in patients with heart failure are coronary artery disease and hypertension. The appropriate management of these predisposing conditions is also an important consideration in controlling heart failure in the community. Identifiable causes of heart failure include aortic stenosis, cardiomyopathy, mechanical defects such as cardiac valvular dysfunction, hyperthyroidism and severe anaemia. Conditions that place increased demands on the heart can create a shortfall in cardiac output and lead to intermittent exacerbation of symptoms. Symptoms of heart failure may occur as a consequence of hyperthyroidism, where the tissues place a greater metabolic demand, or severe anaemia, where there is an increased circulatory demand on the heart. Cardiac output may also be compromised by bradycardia or tachycardia, or by a sustained arrhythmia such as that experienced by patients in atrial fibrillation.
Signs and Symptoms of Chronic Heart Failure

Chronic Heart Failure
- Patients with heart failure may appear pale and their hands cold and sweaty.
- Reduced blood supply to the brain and kidney can cause confusion and contribute to renal failure, respectively.
- Hepatomegaly occurs from the congestion of the gastrointestinal tract, which is accompanied by abdominal distension, anorexia, nausea and abdominal pain.
- Edema affects the lungs, ankles, and abdomen.
- Signs of edema in the lungs include crepitations heard at the lung bases.
- In acute heart failure, symptoms of pulmonary edema are prominent and may be life-threatening.
- The sputum may be frothy and tinged red from the leakage of fluid and blood from the capillaries
Clinical manifestations of heart failure
- Venous (congestion): Dyspnoea, Oedema, Hypoxia, Hepatomegaly, Raised venous pressure
- Cardiac (cardiomegaly): Dilation, Tachycardia, Regurgitation, Cardiomyopathy, Ischemic, arrhythmia
- Arterial (peripheral hypoperfusion): Fatigue, Pallor, Renal impairment, Confusion, Circulatory failure
Diagnosis of Chronic Heart Failure
Four Diagnostic tests are performed to confirm a diagnosis of heart failure.
- Blood test
- 12-lead electrocardiogram
- Chest radiograph
- Echocardiography
Treatment of Chronic Heart Failure
Pharmacotherapy aim is to control symptoms, where diuretics and digoxin are the mainstays of treatment. While relieving the symptoms of heart failure remains decisive in improving a patient’s quality of life, a better understanding of the underlying pathophysiology has led to major advances in the pharmacological treatment of heart failure. With the introduction of angiotensin-converting enzyme (ACE) inhibitors, b-blockers, angiotensin II receptor blockers (ARBs) and aldosterone antagonists, delaying disease progression and ultimately improving survival have become realistic goals of therapy.
Patient Care of Chronic Heart Failure
- Heart failure remains poorly understood by the general public, amongst whom only 3% were able to identify the condition when presented with a list of typical symptoms.
- Patients with heart failure are often elderly and often include patients with comorbidity such as coronary heart disease and hypertension.
- Other complications include renal impairment, polypharmacy and variable adherence to prescribed medication regimens.
- Where the renal function is compromised, careful attention to dosage selection is required for drugs excreted largely unchanged in the urine.
- Patients with heart failure are at particular risk of fluid or electrolyte imbalance, adverse effects, and drug interactions.
- Consequently, careful monitoring is indicated to help detect problems associated with suboptimal drug therapy, unwanted drug effects, and poor patient adherence.
- A number of therapeutic problems may be encountered by the patient with heart failure.
- Notably, heart failure often complicates other serious illness and is a common cause of hospital admission.
- In addition to monitoring clinical signs and symptoms in the acute setting, there should be monitoring of fluid and electrolyte balance, assessment of renal and hepatic function, and performance of chest radiograph, electrocardiograph and hemodynamic measurements where appropriate.













































