Asthma: Incidence, Causes, Diagnosis, Treatment, Patient Care
Asthma Disease
Asthma means ‘laboured breathing’ in Greek and was first described 3000 years ago. It is a broad term used to refer to a disorder of the respiratory system that leads to episodic difficulty in breathing. According to The National (BTS/SIGN) guidelines, asthma is defined as ‘a chronic inflammatory disorder of the airways
Asthma Disease
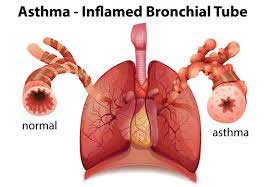
which occurs in susceptible individuals; inflammatory symptoms are usually associated with widespread but variable airflow obstruction and an increase in airway response to a variety of stimuli. Obstruction is often reversible either spontaneously or with treatment’.
Incidence Of Asthma
The exact prevalence of asthma remains uncertain because of the differing ways in which airway restriction is reported, diagnostic uncertainty (especially for children under 2 years) and the overlap with other conditions such as chronic obstructive pulmonary disease (COPD). Over 5 million people in the UK have asthma (Asthma UK, 2001) and around 300 million worldwide. Mortality from asthma is estimated at approximately 0.4 per 100,000 with around 1400 deaths per annum in the UK. Most deaths occur outside the hospital; the most common reasons for death are thought to be an inadequate assessment of the severity of airway obstruction by the patient and/or clinician and inadequate therapy with inhaled or oral steroids.
Causes Of Asthma
The two main causes of asthma symptoms are airway hyperresponsiveness and bronchoconstriction. Hyperresponsiveness is an increased tendency of the airway to react to stimuli or triggers to cause an asthma attack. Bronchoconstriction is a narrowing of the airways that causes airflow obstruction.
Causes Of Asthma
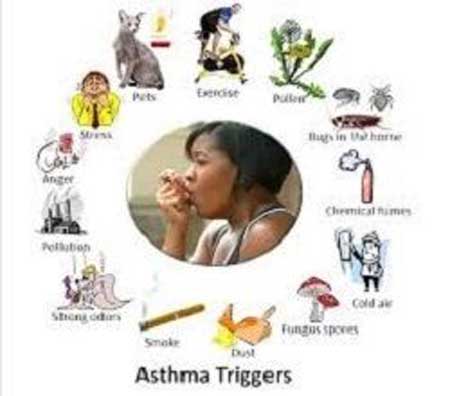
Possible Triggers are listed below:
Possible Triggers are listed below
- Allergens Pollens, molds, house dust mite, animal (dander, saliva, and urine)
- Industrial Chemicals Manufacture of, for example, isocyanate-containing paints, epoxy resins, aluminum, hair sprays, penicillins and cimetidine
- Drugs Aspirin, ibuprofen and other prostaglandin synthetase inhibitors, β-adrenoceptor blockers
- Foods A rare cause but examples include nuts, fish, seafood, dairy products, food coloring, especially tartrazine, benzoic acid and sodium metabisulfite
- Environmental pollutants Traffic fumes. cigarette smoke, sulfur dioxide
- Other industrial triggers Wood or grain dust, colophony in solder, cotton, dust, grain weevils and mites
- Miscellaneous Cold air, exercise, hyperventilation, viral respiratory tract infections, emotion or stress, swimming pool chlorine
Diagnosis of Asthma
The function of the lungs can be measured to help diagnose and monitor various respiratory diseases. A series of routine tests has been developed to assess asthma as well as other respiratory diseases such as COPD.
The most useful test for abnormalities in airway function is the forced expiratory volume (FEV). This is measured by means of lung function assessment apparatus such as a spirometer. The patient inhales as deeply as possible and then exhales forcefully and completely into a mouthpiece connected to a spirometer. The FEV1 is a measure of the FEV in the first second of exhalation. The forced vital capacity (FVC) can also be measured, which is an assessment of the maximum volume of air exhaled with a maximum effort after maximum inspiration. The FEV1 is usually expressed as a percentage of the total volume of air exhaled, reported as the FEV1 /FVC ratio. This ratio is a useful and highly reproducible measure of the capabilities of the lungs. Normal individuals can exhale at least 70% of their total capacity in 1 s. In obstructive lung disorders, such as asthma, the FEV1 is usually decreased, the FVC normal or slightly reduced and the FEV1 /FVC ratio decreased, usually <0.7
Treatment for Asthma
As asthma involves inflammation and bronchoconstriction, treatment should be directed towards reducing inflammation and increasing bronchodilation. Treatment aims should include a lack of day and nighttime symptoms, no asthma exacerbations, no need for rescue medication, normal PEFs and no unwanted side effects from medication (BTS/SIGN). Anti-inflammatory drugs should be given to all but those with the mildest of symptoms. Other measures, such as avoidance of recognized trigger factors, may also contribute to the control of this disease. The lowest effective dose of drugs should be given to minimize short-term and long-term side effects. It should, however, always be remembered that asthma is a potentially life-threatening illness, is often undertreated and not all patients will achieve optimal control.
Reliever medication For Asthma
Short-acting β-adrenoceptor agonist bronchodilators. β-Adrenoceptor agonists are the mainstay of asthma management. Salbutamol and terbutaline are selective β2 -agonists and have few β1 -mediated side effects such as cardiotoxicity. β2 -Receptors are, however, also present in myocardial tissue; cardiovascular stimulation resulting in tachycardia and palpitations is still the main dose-limiting toxicity with these agents when used in high dosage
Management of common practice problems
- Reducing exposure to trigger risk factors may help to improve asthma control.
- Successful management of asthma requires a partnership between the patient and the health care provider.
- Aim to give patients the ability to control their asthma by supporting guided self-management.
- Individualized action plans improve health outcomes, particularly in moderate to severe disease.
- Increased use of reliever medication is a warning of deterioration of asthma control.
- Assessment of asthma control is essential when deciding to step up or step down treatment.
- At each treatment review, inhaler technique and adherence to treatment should be checked.
- The main treatments for exacerbations of asthma include repeated β2 -agonists, early use of corticosteroids and oxygen to raise Sao2 above 92%.
- Mild exacerbations (PEF reduction of <20%) can often be managed in community settings.
- After exacerbations, patients should be reviewed early to identify possible triggers and review the action plan.
Patient care
- The correct use of drugs and the education of patients are the cornerstones of asthma management. There are three main steps in the education of the asthmatic patient.
- The patient should have an understanding of the action of each of the medicines they use.
- The appropriate choice of an inhalation device(s) should be made and the patient educated to use them correctly.
- An individualized action (self-management) plan should be developed for each patient.













































