Arrhythmias: Symptoms, Causes, Diagnosis, Treatment
Arrhythmias
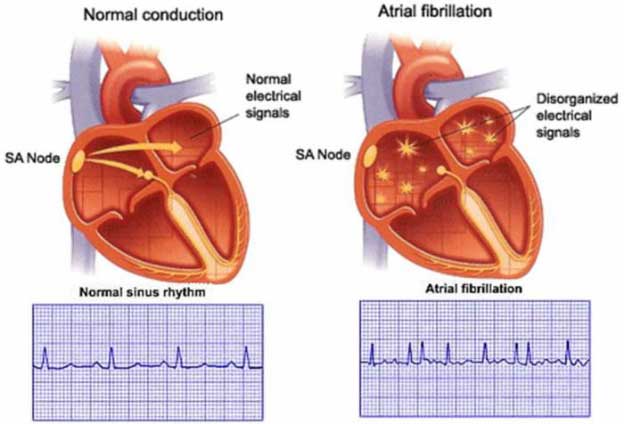
Cardiac arrhythmias occur because of abnormalities of impulse formation or propagation. Abnormal impulse formation
Abnormal Automaticity
Automaticity is another term for pacemaker activity, a characteristic possessed by all cells of the specialised cardiac conduction system during health and, potentially, by other cardiac myocytes during certain disease states. The rate of firing of a pacemaker cell is largely determined by the duration of the phase 4 diastolic interval This in turn is determined by (i) the maximum diastolic potential following depolarization of the preceding action potential, (ii) the slope of diastolic depolarisation due to pacemaker currents and (iii) the threshold potential for generation of a new action potential. In the healthy state, there is a hierarchy of firing rates within the specialised conduction system with the highest rate in the sinus node followed by the AV node and then the His–Purkinje system.
Arrhythmias
Abnormal Impulse Propagation
Re-entry
Many clinically important arrhythmias are due to reentry, in which an activation wavefront rotates continuously around a circuit. Re-entry depends upon a trigger in the form of a premature beat, and a substrate, that is, the reentry circuit itself.
Signs And Symptoms of Arrhythmias
Patients with a cardiac arrhythmia may present with a number of symptoms:
The most common symptom is palpitation, an awareness of an abnormal heartbeat, although some patients with clearly documented arrhythmia have no palpitation. Arrhythmias start suddenly and, therefore, if the patient clearly describes palpitation of sudden onset (‘like flicking a switch’), this is a useful pointer to an arrhythmia rather than heightened awareness of sinus tachycardia, which has a less sudden onset.
The heart is designed to work most efficiently in sinus rhythm. Any arrhythmia compromises cardiac function. Classical symptoms that arise due to reduced cardiac output include reduced exercise capacity, breathlessness and fatigue.
Angina may accompany tachycardia, even in the absence of coronary artery disease. Tachycardia increases the metabolic rate of cardiac muscle and hence its demand for blood flow. Myocardial perfusion occurs predominantly during diastole and during tachycardia proportionately less time is spent in diastole and so myocardial demand for blood can exceed supply, resulting in angina.
A sudden drop in cardiac output may accompany either bradycardia or tachycardia, causing episodes of dizziness (presyncope), loss of consciousness (syncope) or, in extreme cases, sudden death from cardiac arrest.
Atrial tachyarrhythmias such as atrial flutter and atrial fibrillation may be complicated by the development of intracardiac thrombus, usually within the left atrial appendage. This thrombus may embolize to any part of the body but the most common clinical presentation is with a transient ischaemic attack or stroke. Arrhythmias may aggravate heart failure in two ways: (i) the haemodynamic effect of the arrhythmia may precipitate heart failure or aggravate existing heart failure and (ii) prolonged tachycardia of any type may lead to tachycardia-induced cardiomyopathy
Diagnosis of Arrhythmias
It includes a 12-lead ECG and an echocardiogram to detect structural heart disease. Other investigations for structural and ischaemic heart disease may be indicated at this stage with the aim of detecting any underlying structural heart disease. If the history does not include sinister features such as syncope or a family history of sudden unexpected death at a young age, and the resting 12-lead ECG and echocardiogram are normal, then the patient can be reassured that they are extremely unlikely to have a serious heart rhythm disturbance. The extent of further investigation will be dictated by how troublesome the symptoms are.
Treatment for Arrhythmias
Management
Cardiac arrhythmias associated with unstable angina, heart failure or hypotension requires emergency treatment. In most cases, the treatment of choice is d.c. cardioversion.
Concerns about thromboembolism as the heart returns to sinus rhythm are valid but should not delay emergency treatment. Immediate d.c. cardioversion is appropriate when the onset of arrhythmias is clearly identified as within 48 h of presentation or when the patient is already taking warfarin and has had a therapeutic INR for at least 4 weeks.
If facilities permit, a transesophageal echocardiogram may be performed in patients not already on warfarin in order to exclude intracardiac thrombus. Heparin should then be given immediately and continued until the INR is within the therapeutic range.
Anticoagulant therapy should be continued for at least 3 months following cardioversion. Long-term stroke prophylaxis is guided thereafter by the CHADS2 score.
If d.c. cardioversion is deemed inappropriate, rapid ventricular rate control may be achieved with intravenous ß-blockers, verapamil or digoxin.
Drug Therapy for Arrhythmias
Antiarrhythmic drug therapy is used to control the frequency and severity of arrhythmias, with the aim of maintaining sinus rhythm where possible. Although antiarrhythmic drug treatment has been the mainstay of arrhythmia treatment, many of these drugs have limited efficacy and important toxicity. Many arrhythmias are now curable by catheter ablation. Implantable devices such as permanent pacemakers and ICDs have assumed an increasingly important role in the treatment of arrhythmias and, in many cases, antiarrhythmic drugs have an adjunctive role.
















































